Varicose veins are swollen, twisted veins that are visible just under the surface of the skin. They are usually formed in the legs, but can also be found in other parts of the body. Varicose veins form when the veins in the legs are not functioning properly and are not able to efficiently pump blood back to the heart. This can cause blood to pool in the veins, leading to their characteristic swelling and twisting appearance. Varicose veins are a common condition, affecting up to 15% of the adult population. While they are usually harmless, they can cause discomfort and can sometimes lead to more serious health problems.
Varicose veins are more common in women than in men, and the prevalence increases with age. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), about 25% of women and 20% of men have varicose veins by the age of 50. The likelihood of developing varicose veins also increases with certain risk factors, such as genetics, obesity, prolonged standing or sitting, hormonal changes during pregnancy, and aging.
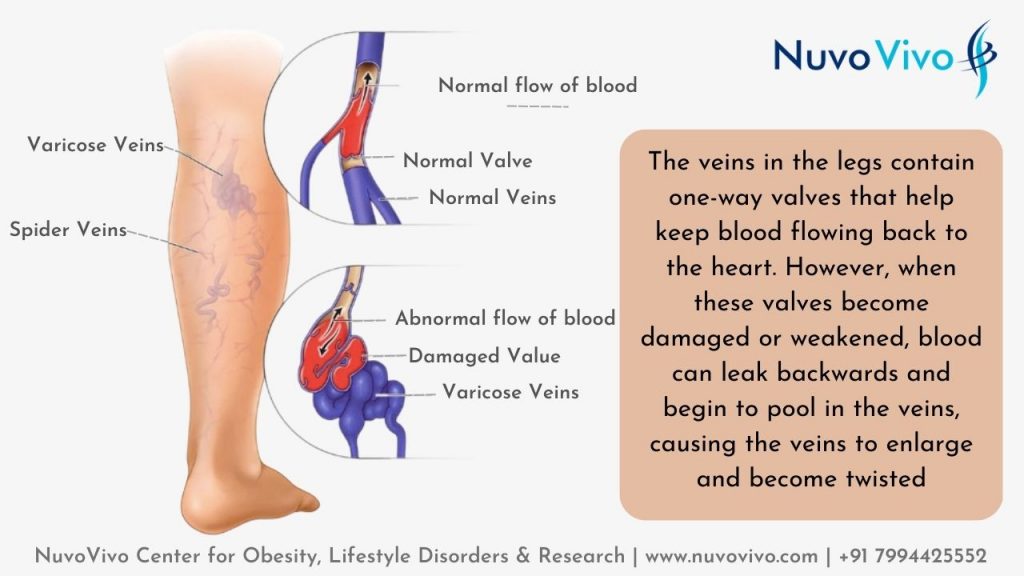
Cause of Varicose Vein
People get varicose veins because the veins in their legs are not functioning properly. Normally, the veins in the legs contain one-way valves that help keep blood flowing toward the heart. However, when these valves become damaged or weakened, blood can leak backwards and begin to pool in the veins. This can cause the veins to enlarge and become twisted, resulting in the characteristic appearance of varicose veins.
Some of the factors that can contribute to the development of varicose veins are:
- Age: The risk of developing varicose increases with age as the veins and valves in the legs become weakened over time.
- Genetics: Some people have a genetic predisposition to develop varicose veins, meaning that the condition can run in families. The link between genetics and varicose veins is well established. Studies have identified specific genes that may increase the risk of developing varicose veins, including those that regulate the structure and function of blood vessels, as well as those that control the contraction and relaxation of blood vessels. In addition, researchers have identified genetic mutations that are associated with a higher risk of developing varicose veins, as well as other venous disorders such as deep vein thrombosis (DVT). While genetics may play a role in the development of varicose veins, it is important to note that the condition can also be caused by other factors, such as obesity, a sedentary lifestyle, and hormonal changes. Additionally, even if a person has a family history of varicose veins, they may not necessarily develop the condition themselves. Overall, the link between genetics and varicose veins highlights the importance of maintaining good vein health and taking steps to reduce the risk of developing the condition, regardless of one’s family history. This can include maintaining a healthy weight, avoiding standing or sitting for long durations, and exercising regularly
- Hormonal changes: Hormonal changes, such as those that occur during pregnancy, can increase the risk of developing varicose veins.
- Pregnancy: pregnancy can be a cause of varicose veins. During pregnancy, hormonal changes can cause the veins to relax and enlarge, making it more difficult for the blood to flow back to the heart. The increased blood volume and pressure in the blood vessels can also lead to the formation of this condition. Additionally, the growing uterus can put pressure on the blood vessels in the legs, further contributing to the development of varicose veins. It’s estimated that about half of all pregnant women develop this condition, although the condition usually improves after giving birth. In some cases, however, it can persist even after pregnancy and may require treatment. It’s important for pregnant women to be mindful of their vein health and to take steps to prevent the development of varicose veins, such as maintaining a healthy weight, avoiding prolonged standing or sitting, and exercising regularly
- Sedentary lifestyle: Prolonged sitting or standing can put extra pressure on the veins in the legs and increase the risk of developing varicose veins.
- Obesity: Excess weight can put additional pressure on the veins in the legs, increasing the risk of developing varicose veins.
Overall, varicose veins are a complex condition that can be caused by a combination of factors.
Symptoms of Varicose Veins
The symptoms can vary depending on the severity of the condition. Some common symptoms include:
- Visible veins: Varicose veins are typically visible just under the skin, appearing as swollen, twisted, and rope-like veins.
- Leg swelling: Some people may experience swelling in their legs, especially after prolonged standing or sitting.
- Leg pain: Some people may experience aching, cramping, or pain in the legs.
- Leg fatigue: People with varicose veins may also experience a feeling of heaviness or fatigue in their legs.
- Skin changes: In some cases, varicose veins can cause the skin over the veins to become discoloured, thick, or dry.
- Restless legs: Some people may experience restless legs syndrome, a condition characterized by an irresistible urge to move the legs.
It’s important to note that not everyone with varicose veins may experience symptoms. In some cases, the condition may be asymptomatic and will only be detected through a routine physical examination.
Also Read: Managing Hypertension through lifestyle changes
Diagnosis of Varicose Veins
The diagnosis of varicose veins typically begins with a physical examination by your doctor. During the exam, your doctor will look for visible signs of varicose veins, such as swollen, twisted, and rope-like veins just under the skin.
In addition to a physical exam, your doctor may also use one or more of the following diagnostic tests to confirm the diagnosis of this condition:
- Duplex ultrasound: This is a non-invasive test that uses sound waves to create images of the veins. The test can help your doctor assess the flow of blood through the veins and determine if there are any blockages or valves that are not functioning properly.
- Venography: This is a more invasive test that involves injecting a dye into the veins and taking X-rays to visualize the veins. The test can help your doctor assess the flow of blood through the veins and identify any abnormalities.
- Magnetic resonance imaging (MRI): This is a non-invasive test that uses a strong magnetic field and radio waves to create images of the veins. The test can help your doctor assess the flow of blood through the veins and identify any blockages or valves that are not functioning properly.
Based on the results of the physical exam and diagnostic tests, your doctor will be able to diagnose and determine the best course of treatment.
Also Read: Diet & Exercise for Heart Health
Treatment Options for Varicose Veins
The treatment options for varicose veins will depend on the severity of the condition and the presence of any symptoms. In some cases, simple lifestyle changes and compression stockings may be all that is needed to manage the disease. In other cases, more aggressive treatments may be required. Here are some of the common treatments –
- Lifestyle changes: Making simple changes in lifestyle, such as maintaining a healthy weight, avoiding prolonged standing or sitting, and exercising regularly, can help improve circulation and reduce the risk of developing varicose veins.
- Compression stockings: Wearing compression stockings can help improve circulation and reduce swelling in the legs. The stockings apply gentle pressure to the legs and help keep blood from pooling in the veins.
- Sclerotherapy: Sclerotherapy is a minimally invasive procedure used to treat varicose veins. During the procedure, a solution is injected into the affected veins, causing them to collapse and eventually disappear. Sclerotherapy is usually performed on an outpatient basis and hence does not require a GA (General Anesthesia). The procedure is highly effective in treating minor to medium-sized varicose veins and can provide significant relief of symptoms such as pain, swelling, and leg fatigue.
- Endovenous laser treatment (EVLT): Endovenous laser treatment (EVLT) is a minimally invasive procedure used to treat varicose veins. During the procedure, a laser is inserted into the affected veins and used to heat and close off the vein. EVLT is typically performed on an outpatient basis and under local anesthesia, with patients able to return to normal activities within a few days. This treatment is highly effective in treating larger varicose veins and can provide significant improvement in symptoms such as pain, swelling, and leg fatigue. It’s also less invasive and has a shorter recovery time compared to traditional vein-stripping surgery
- Ambulatory phlebectomy: Ambulatory phlebectomy is a minimally invasive procedure used to treat varicose veins. During the procedure, small incisions are made in the skin and the affected veins are removed through the incisions. The procedure is performed on an outpatient basis and under local anesthesia, with patients able to return to normal activities within a few days. Ambulatory phlebectomy is highly effective in treating small to medium-sized varicose veins and can provide significant relief of symptoms such as pain, swelling, and leg fatigue.
- Vein ligation and stripping: Vein ligation and stripping is a surgical procedure used to treat varicose veins. During the procedure, the affected veins are tied off and removed through small incisions in the skin. The procedure is typically performed under general anesthesia and is usually reserved for more severe cases of varicose veins. Vein ligation and stripping are highly effective in treating larger varicose veins and can provide significant improvement in symptoms such as pain, swelling, and leg fatigue. However, it does have a longer recovery time compared to minimally invasive procedures like sclerotherapy or endovenous laser treatment (EVLT)
It’s important to speak with your doctor or vascular surgeon to determine the best course of treatment for your individual needs. In many cases, a combination of the above treatment protocols may be recommended by your doctor. The goal of treatment is to relieve symptoms, improve circulation, and prevent the progression of the condition
Also Read: Creatinine & Kidney Health
Prevention of Varicose Veins
While it may not be possible to completely prevent the development of varicose veins, there are steps you can take to reduce your risk of developing this condition:
- Exercise regularly: Regular physical activity, such as walking, running, swimming, or cycling, can help improve circulation and reduce the risk of developing varicose veins.
- Maintain a healthy weight: Being overweight or obese can increase the pressure on your veins and increase your risk of developing this condition. Maintaining a healthy weight can help reduce this risk.
- Avoid prolonged standing or sitting: Prolonged standing or sitting can cause blood to pool in your veins, leading to the development of varicose veins. Taking regular breaks and moving around can help improve circulation and reduce the risk of developing it.
- Wear compression stockings: Compression stockings can help improve circulation and reduce swelling in the legs. They apply gentle pressure to the legs and help keep blood from pooling in the veins.
- Raise your legs: Raising your legs above your heart level can help improve circulation and reduce swelling in your legs. This can be done by simply lying down and placing a pillow under your feet.
- Avoid tight clothing: Tight clothing, such as tight pants or socks, can restrict circulation and increase the risk of developing varicose veins. Wearing loose-fitting clothing can help improve circulation and reduce the risk of developing varicose veins.
- Manage constipation: Constipation can increase the pressure on your veins and increase your risk of developing this condition. Eating a high-fiber diet and staying hydrated can help reduce the risk of constipation and improve circulation.
Also Read: Breathing to manage Stress
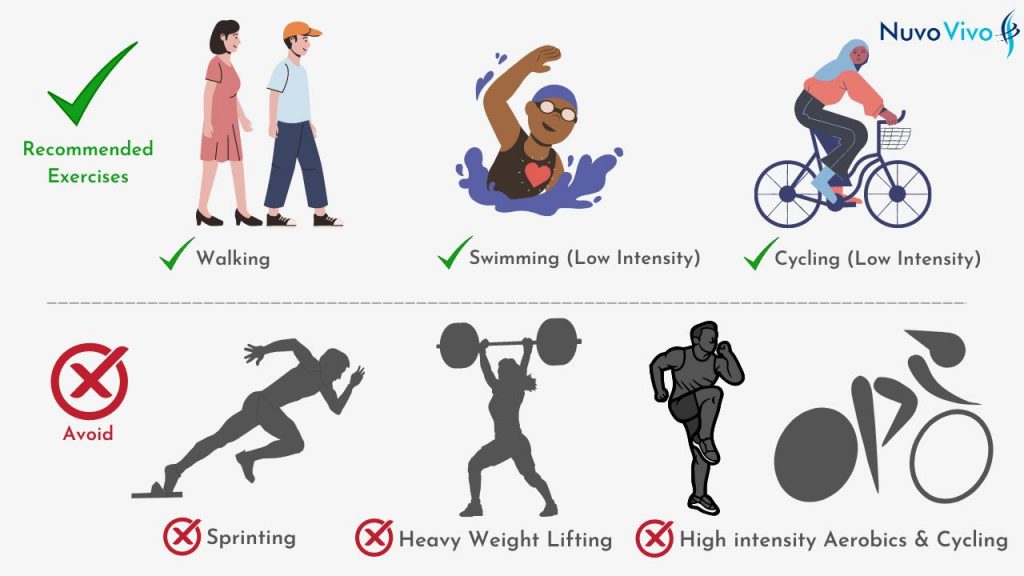
Exercise for Varicose Veins – Dos & Don’ts
Exercise is important for improving circulation and reducing the risk of developing varicose veins. Some of the most suitable exercises for people with varicose veins include:
- Walking: Walking is a low-impact exercise that can help improve circulation and reduce the risk of developing varicose veins.
- Swimming: Swimming is a great exercise for people with varicose veins as it helps improve circulation and provides a full-body workout.
- Cycling: Cycling is another low-impact exercise that can help improve circulation and reduce the risk of developing varicose veins.
It’s important to avoid exercises that put a lot of pressure on your legs, such as heavy weightlifting or high-impact aerobics, as these can increase the risk of developing varicose veins.
Also Read: Different types of Exercises
When engaging in exercise, it’s important to:
- Wear comfortable, supportive shoes: Wearing shoes that provide good support can help reduce the risk of developing varicose veins.
- Stay hydrated: Staying hydrated can help improve circulation and reduce the risk of developing varicose veins.
- Stretch before and after exercise: Stretching before and after exercise can help reduce the risk of developing varicose veins by improving circulation.
It’s also important to avoid:
- Prolonged standing or sitting: Prolonged standing or sitting can increase the risk of developing varicose veins, so it’s important to take regular breaks and move around.
- Wearing tight clothing: Wearing tight clothing, such as tight pants or socks, can restrict circulation and increase the risk of developing varicose veins, so it’s important to wear loose-fitting clothing.
About NuvoVivo
NuvoVivo is an online health and fitness company that helps its client manage lifestyle diseases. Our clients join us from across the world to manage or reverse conditions such as diabetes (and its complications), cardiovascular diseases (hypertension, high cholesterol), fatty liver, PCOS, thyroid disorders, IBS etc. We help them reduce their reliance on medications through structured and scientific lifestyle changes that suit their cultural habits and medical conditions. Our team provides a diet plan, exercise plans and the necessary follow-up and support in helping them achieve this
Reach for Consultations @ https://bit.ly/NVConsultation
More about NuvoVivo @ https://linktr.ee/nuvovivo

This Post Has One Comment
Such a useful post. It explains everything … enlightening us…and removes all the misconceptions about Varicose. Thank u