Have you ever experienced the unpleasant feeling of discomfort, itching, irritation, or pain in the anal region while sitting or during bowel movements?
If yes, it could be a warning sign that you are suffering from an underlying condition called piles. Piles or Hemorrhoids (in medical terminology) are a common but rarely talked about problem.
Sometimes, they are an occasionally fleeting rectal discomfort and often go away on their own devoid of treatment. But, if you are suffering from ongoing pain or severe itching or bleeding, you should seek medical attention.
People often feel ashamed and embarrassed about hemorrhoids and are reluctant to talk about this problem even to their healthcare providers. You are not alone, don’t shy away from discussing the symptoms of piles with your doctor.
Millions of people are affected with hemorrhoids at some point in their lives, corresponding to an estimated prevalence rate of 4.4% worldwide.
This article will discuss what piles disease is, the symptoms of piles, causes of piles, types of hemorrhoids, treatment for hemorrhoids, and much more. Are piles dangerous? Are piles painful? Or how to cure piles? Scroll down and keep reading to get answers to all these questions popping into your mind right now.
Hear our podcast on Piles and Fistula.
What are Piles (Hemorrhoids)?
The swollen veins located in the lower rectum and around the anus are referred to as piles or hemorrhoids.
This can usually develop due to prolonged sitting or straining to have bowel movements caused by long-term constipation.
Anal blood vessels are part of the normal rectum and anal canal anatomy, which help you maintain bowel continence. But piles can happen if these blood vessels are dilated and engorged with blood more than normal.
At what age piles can occur is a frequent doubt asked by a lot of people. Even though people can get hemorrhoids at any age, adults between the ages of 45 and 65, as well as pregnant women, are more likely to develop this condition.
Typically, the signs of piles are not that obvious for many people. But symptomatic hemorrhoids can sometimes cause severe pain and rectal bleeding that may lead to infection, making it crucial to visit a doctor during the initial stages.
Different Types of Hemorrhoids
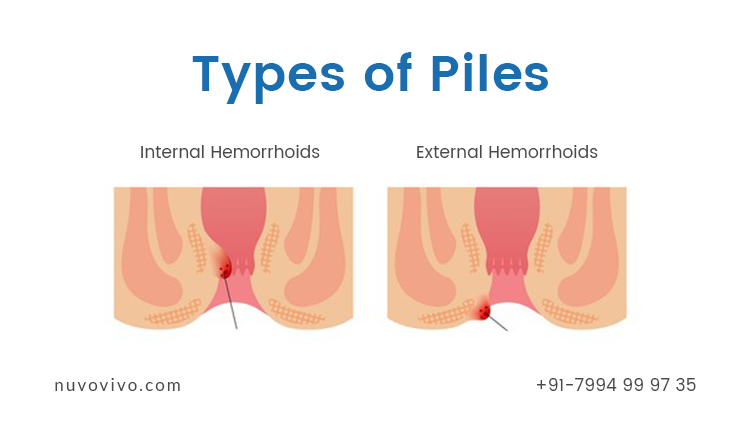
Based on where the swollen vein happens, inside or outside, in the rectum, the hemorrhoids are mainly classified into two types – internal piles and external piles.
1. Internal Hemorrhoids
Internal hemorrhoids happen when the veins on the inside lining near the end of the rectum are swollen. They develop deep inside the rectum. Unless they are prolapsed, you can’t see or feel internal hemorrhoids.
As they are located in an area with only a few pain-sensing nerves, these types of hemorrhoids usually are painless. Sometimes, excessive straining during the bowel movement can push the internal piles, which can cause prolapsed hemorrhoids.
Internal piles are further classified into four different grades depending on the degree of prolapse and its severity. These grading from scale I to IV helps in guiding effective treatment. Each grade can cause diverse signs and symptoms.
Grade I
These types of internal hemorrhoids are not visible and can’t be felt as they are small swellings located on the inside lining of the rectum and not prolapsed at all.
Grade II
Grade II internal hemorrhoids are larger than grade I. These types of internal hemorrhoids may only prolapse or be pushed out due to straining during the bowel movement.
Even though these internal piles are prolapsed, they can naturally go back inside on their own once the straining has subsided.
Grade III
Prolapsed hemorrhoids that protrude outside the anal canal are referred to as grade III internal piles. These types of hemorrhoids don’t retract themselves, but they can be receded by gently pushing them back in.
Grade III internal hemorrhoids are often accompanied by itching and soilage. Even though these are not the most severe internal piles, medical treatment may be needed so that they don’t turn out to be excessively painful or infected.
Grade IV
Grade IV internal hemorrhoids are large, irreducible, and remain prolapsed outside the anus. They can’t be pushed back inside the anus. These types of internal piles usually co-occurred with chronic local inflammatory changes and need immediate treatment to avoid further pain, discomfort, and other potential complications.
2. External Hemorrhoids
The swollen veins beneath the skin around the anus are referred to as external piles. This type of hemorrhoids covered by well-innervated anoderm can cause significant pain than internal piles due to the presence of several pain-sensing nerves there.
External hemorrhoids normally happen due to increased intra-abdominal pressure that occurs in situations like straining with bowel movement, prolonged sitting on the toilet, passing hard stools, and even pushing and straining during child labor. People can often feel external piles if they swell up.
3. Thrombosed Hemorrhoids
When a blood clot develops inside either an internal or external hemorrhoid, thrombosed hemorrhoids happen.
They are also known as acute hemorrhoidal disease or perianal thrombosis. These painful swellings of anal tissues appear as a dark bluish lump if it is acutely thrombosed.
As the blood clot obstructs the blood flow, these types of swellings can be too excruciating.
Usually, the blood clot in these types of piles is reabsorbed by the body, and the signs may go away on their own within two to three weeks, even without any treatment. If the signs and symptoms persist, these should need to be treated to ward off pain, discomfort, or further complications.
Symptoms of Piles

Depending upon the severity and types of hemorrhoids, the symptoms of piles may vary. There is a range of signs and symptoms that can affect an individual with piles, but these are not dangerous in most cases, and many people don’t even have any symptoms at all. Usually, they cure on their own within a few days.
People suffering from external hemorrhoids may have the following symptoms:
- Rectal bleeding (blood in the stool)
- Irritation or itching around the anus or rectal area
- Anal discomfort (pain around the anus, especially when you sit)
- Anal swelling
- Mucus discharge from the anus
People with internal hemorrhoids may experience these symptoms:
- Painless rectal bleeding with a bowel movement. You might see blood on the toilet bowl or in your stool in small amounts and in bright red color or notice it on toilet paper after you wipe.
- At times, internal piles prolapse outside the anus, causing pain and irritation from swelling and itching.
People with thrombosed hemorrhoids can result in symptoms including:
- Hard lump near or around the rim of the anus that may be itchy or painful
- Severe pain or discomfort
- Swelling near the anus
Above are the common piles’ symptoms; however, more severe hemorrhoids can result in more debilitating symptoms, including excessive rectal bleeding that could lead to complications like anemia, anal incontinence, infection, blood cot, and anal fistula.
Causes of Piles
As we discussed earlier, there are different types of piles and no single cause. But, increased pressure in the lower rectum is the root cause of developing hemorrhoids.
If the veins in the lower rectum and anus are constantly under pressure, they tend to become swollen and enlarged, causing piles. The common causes of hemorrhoids include:
- Repeated straining while having a bowel movement
- Prolonged sitting on the toilet
- Passing hard stools
- Increased pressure on the pelvis due to weight gain, especially during pregnancy
- Chronic constipation or diarrhea
- Heavy weight lifting
The other lifestyle risk factors that can develop piles more likely include physical inactivity, dehydration, and a low-fiber diet, as these can contribute to constipation, which can lead to piles.
Treatment for Hemorrhoids
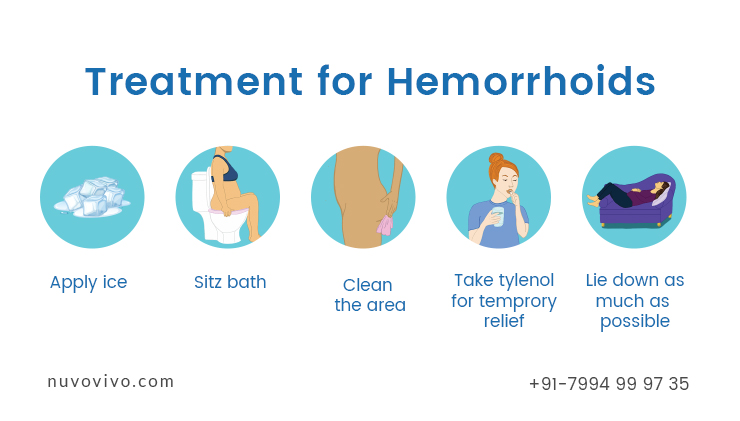
Most of the time, piles can get better on their own without any treatment. Home remedies and lifestyle changes may also help alleviate the symptoms of hemorrhoids within a few days if they are mild.
Exercising, drinking plenty of fluids, and eating fiber-rich food can help reduce the chances of constipation, and thereby, you can avoid the need of straining during bowel movements that can cause hemorrhoids.
Also, try not to push too hard during bowel movements and avoid sitting for extended periods on the toilet as these actions can increase pressure on the anus veins.
But in severe cases, surgical and non-surgical treatments are required to relieve the symptoms and cure piles. The doctor’s treatment plan will vary depending upon the type, degree of prolapse, or severity of your piles’ symptoms.
Non-Surgical Treatments for Piles
Numerous medicinal options are available to make the pain, swelling, itching, and other symptoms more tolerable for people suffering from piles. The medications for treating hemorrhoids include:
- Over-the-counter (OTC) medications, including creams, ointments, suppositories, painkillers, and cold packs, can help to alleviate the symptoms.
- Corticosteroids can be used to reduce pain by lowering inflammation.
- Laxatives can be used to treat constipation.
The non-surgical treatment for piles includes:
- Rubber band ligation: This is a most common non-surgical treatment for hemorrhoid removal in which the protruding piles mass is tied off at its base using a rubber band to hamper the blood supply to the tissue. As the blood flow stops to the hemorrhoid mass, it will shrink and drop off within a week.
- Sclerotherapy: In this treatment, a chemical solution will be administered into the area around the hemorrhoids through an anoscope, which causes scar tissue that cuts off the blood flow to the piles. Eventually, the hemorrhoids shrink and shrivel up over time (about 4 to 6 weeks after treatment).
- Electrotherapy: An electric current is applied to each hemorrhoid in order to cauterize the piles at its base. This procedure is also known as electrocoagulation.
- Infrared coagulation: This non-surgical process, also known as coagulation therapy, treats small- and medium-sized piles. A powerful beam of infrared light is used to scar the tissue, thereby stopping the blood supply to the hemorrhoids, making them shrink.
Surgical Treatments for Piles
If the home remedies and non-surgical treatment options are not helping to get better, then you might require surgical treatment, especially if your piles are too painful, large, or bleeding.
For long-term cure, surgery is the best treatment for hemorrhoids. The surgical treatments for piles include:
- Hemorrhoidectomy
- Stapled Hemorrhoidopexy (Prolapse and Hemorrhoids)
- Hemorrhoidal Artery Ligation and Recto Anal Repair (HAL-RAR)
Piles can be annoying, painful, and uncomfortable. But, generally, the chances of noticeable signs and symptoms are rare, and even if the piles are symptomatic, in most cases, they may go away on their own without any treatment.
Even simple lifestyle changes can help in relieving the symptoms of piles. Hemorrhoids are a common condition, so don’t feel embarrassed to seek medical help if needed.
Diet for Hemorrhoids

The diet for a person with piles (hemorrhoids) should have adequate fiber without excessive fat and protein. This is to facilitate proper digestion and bowel movement.
Including fruits and vegetables in the diet will help in increasing the fiber content in the diet. Dietary fiber is an integral part of digestive and gut health. Most of the dietary fiber passes through our digestive system without being digested or broken down.
However, they help in many other ways – including improving bowel movements, regularizing bowel movements, improving digestion, controlling blood sugar, cholesterol, etc.
There are two types of dietary fiber, viz. soluble fiber, and insoluble fiber. Soluble fiber, as the name says, can dissolve in water. Examples are pectin, gums, etc. On the other hand, insoluble fiber does not dissolve in water.
Examples are cellulose and hemicellulose. Insoluble fiber is particularly helpful in binding the stool and making it softer, thereby allowing better bowel movement and letting the stool pass without much strain.
Apart from improving gut health, it can help in regularizing bowel movements.
Apart from including dietary fiber, reduce caffeine intake. Alcohol and smoking can also impair digestion and gut health and are best avoided.
Including too much protein and fiber can sometimes cause constipation and may further exacerbate inflammation and pain. Adequate water intake is yet another important factor for proper digestion and bowel movement.
Exercises for Hemorrhoids
Reducing excessive body weight is very important to manage piles. Exercises, however, need to be done such that it does not make the piles worse!
For example – strenuous weight training that involves a lot of core muscles can make piles worse. Compound exercises that involve a lot of core engagement, such as squats, weighted squats, etc., are best avoided. Also, avoid high-intensity exercises and abdominal exercises.
Exercises that will strengthen the pelvic floor muscles are particularly helpful in managing piles. Pelvic floor muscles are dome-shaped muscles that support the pelvic organs, such as the urinary bladder and uterus (for women). When pelvic floor muscles are weakened, it can cause bladder and bowel control issues and even piles.
Pelvic floor muscles in men have the urethra (the tube that passes urine) and anus passing through it, while women have the uterus also passing through it.
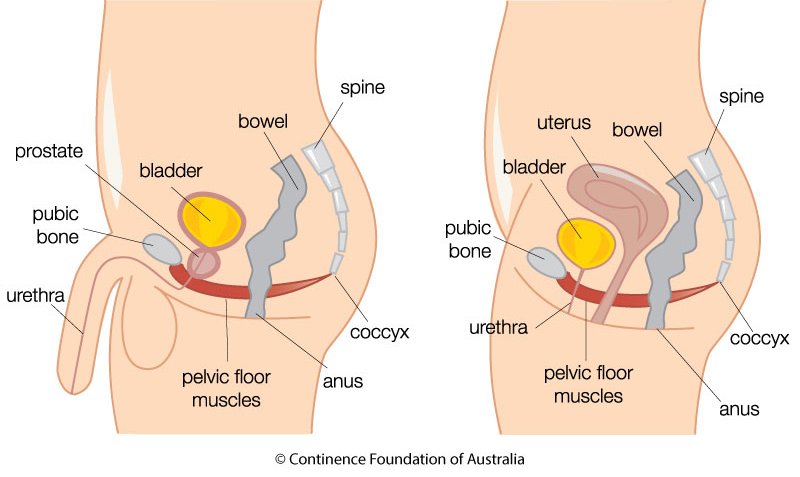
This is the reason why women are prone to piles after pregnancy, as the pelvic floor muscle may become weak, especially after vaginal birth. Strengthening the pelvic floor muscles is hence helpful in managing piles.
Kegel Exercise for Pelvic floor muscles
Kegel exercise is helpful in strengthening the pelvic floor muscles. Lie down on a flat surface and gently lift the abdomen (as seen in the image below) while contracting/squeezing the pelvic floor muscles.
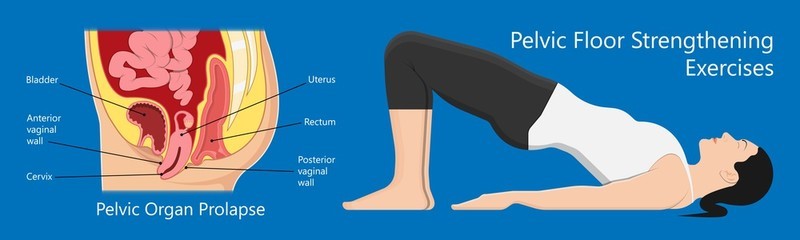
Be cognizant that you are engaging pelvic floor muscles and not just the abdomen or the glutes.
One easy method to feel/engage the pelvic floor muscles is to try squeezing and releasing the anal sphincter muscles (muscles at the opening of the anus) without engaging the muscles on the butt (glutes) or the abdomen.
NuvoVivo is an online health, wellness & fitness center that is into medical fitness & lifestyle management. We specialize in transformation (weight loss, muscle gain) and also in managing lifestyle conditions such as diabetes management, cholesterol, thyroid, PCOD and PCOS management, fatty liver, uric acid, hypertension, etc through nutrition & exercises. Our programs are all online, and our clients are from across the world to manage such lifestyle disorders, lose weight, etc. For more details, Contact us at +91 79949 99914


This Post Has One Comment
Amazing article,detailed and informative👍